The health insurance industry's lobbying muscle in the California Legislature is legendary. It's the reason that the state's insurance commissioner remains all but toothless to reject outrageous spikes in health insurance premiums and rates, unlike in a majority of other states. So it's not a shock that a new version of a bill to let the state insurance commissioner reject or modify health insurance premiums barely squeaked through the state Assembly's Appropriations Committee late last week with the minimum 9 votes.
The health insurance industry's lobbying muscle in the California Legislature is legendary. It's the reason that the state's insurance commissioner remains all but toothless to reject outrageous spikes in health insurance premiums and rates, unlike in a majority of other states. So it's not a shock that a new version of a bill to let the state insurance commissioner reject or modify health insurance premiums barely squeaked through the state Assembly's Appropriations Committee late last week with the minimum 9 votes.
+++Take Action Here to Cut Insurance Premiums, Send a Message to Your Legislator+++
The bill will face another firestorm of industry lobbying when it comes up for a full Assembly vote in a few days.
This legislation ought to be a slam dunk, after Blue Shield tried to jam through premium increases of up to 86% in a single year. Aetna and Blue Cross weren't much better. The only reason any insurer backed down even a little was because of public rage, which is not a good regulatory tool in the long run. When every Californian is required to show proof of insurance as of 2014, Californians will be even more in need of protection from insurance industry greed. And nearly every major newspaper has supported health insurance regulation–the LA Times made its second strong editorial argument Tuesday. (text of editorial is below)
So what was up with the two Democrats–Charles Calderon and Jose Solorio–who voted against the rate regulation bill (AB 52, Mike Feuer)? First they reportedly tried to get author Feuer to accept last-minute substantive changes without a chance to examine what they meant–and Feuer rightly refused. Then Calderon and Soloio voted no. Hmm. Solorio is among the top five recipients of insurance industry money in the Assembly. And Calderon is the sponsor of a bill (AB 736)–strongly supported by the health insurance insurance and broker industries–that would remove consumer protections from health broker misdeeds or errors and indirectly raise health insurance premiums.
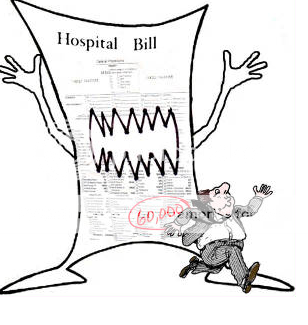
Two million Californians lost their insurance during the recession, bringing the state's total uninsured to 8 million. From the mail we get, a whole lot of people are right on the edge of having to drop Health insurance. It's long past time for the largest state in the nation to get a grip on health insurance spikes in the high double digits, even as overall medical inflation sinks to around 4% a year. Something is wrong with this picture, even if it's just right for insurance companies' record profits.
We hope Calderon and Solorio were just making a procedural protest and that they'll protect consumers, not insurance company profits, when the Assembly votes this week on AB52. It'll be close. Here's the button to Take Action.
A lid on health insurance rate increases
California regulators should be given the power to reject unreasonable increases in health insurance premiums.
May 31, 2011
Opponents of a bill that would allow state regulators to reject unreasonable increases in health insurance premiums are stepping up their attacks on the measure, contending that it would push premiums even higher and make healthcare less available. These arguments are a smokescreen, and lawmakers shouldn't lose sight of the need to give consumers of health insurance the same protection they have in auto and homeowners' policies.
One allegation is that the bill — AB 52, sponsored by Rep. Mike Feuer (D-Los Angeles) — would enrich the consumer advocates who challenge proposed rate increases. That charge is based on the bill's requirement that insurers cover the "reasonable" fees and costs incurred by advocates who make a "substantial contribution" to the ruling by regulators or the courts. The same perfectly sensible language is in Proposition 103, the initiative that empowered state regulators to reject excessive automobile, property and casualty insurance rates.
Giving consumers the opportunity to participate in rate reviews is a valuable counterweight to the shifting policies in Sacramento, where regulators' zeal often depends on who won the last election. And the "substantial contribution" requirement for getting fees reimbursed deters frivolous challenges. Consumer Watchdog, an advocacy group, says its interventions have reduced insurers' proposed auto, home and earthquake premiums by more than $2 billion since 2000; insurers have had to spend an additional $5 million to cover the consumer group's expenses.
Smaller premium increases might seem like a good thing to consumers, but evidently doctors and hospitals feel differently. Their trade associations are opposing AB 52, arguing that it could artificially reduce the rates insurers pay them. Such reductions, they say, could persuade more providers not to take Medicare and Medi-Cal patients because they count on reimbursements from private insurers to cover some of the cost of government-insured patients. But those cross-subsidies are precisely the sort of distortions and inefficiencies that policymakers should be trying to eliminate from the healthcare system, not prop up.
The healthcare reform law Congress passed last year tries to combat cross-subsidies, and it limits insurers' profit margins by tying them to the amount spent on medical care. That link, however, gives insurers a perverse incentive to grow their profits by inflating the amounts they pay doctors and hospitals. That's a good reason to give state regulators the power not just to review rates, as California law now provides, but to reject them when they're unreasonable. Here's another: As of 2014, the healthcare reform law will require all adult Americans to obtain health coverage. Regulators ought to have the power to stop insurers from gouging that captive market.
————-
Posted by Judy Dugan, research director for Consumer Watchdog, a nonpartisan, nonprofit organization dedicated to providing an effective voice for taxpayers and consumers in an era when special interests dominate public discourse, government and politics. Visit us on Facebook and Twitter.